The Beth Israel Deaconess Medical Center Neuro-Oncology Fellowship is designed to nurture the development of future leaders in Neuro-Oncology and provide a supportive environment for clinical and research training. Expert faculty members in Neuro-Oncology, Neurosurgery, Radiation Oncology, Neuropathology, and Neuroradiology work with fellows as instructors, mentors, and future colleagues. The goal of the program is to cultivate future neuro-oncologists who will devote their careers to patient care, teaching, and clinical, translational, or basic research.
The Neuro-Oncology Fellowship offers one two-year United Council for Neurologic Subspecialties (UCNS) approved fellowship per academic year. Fellows will be trained in the management of primary and metastatic central and peripheral nervous system neoplasms, neurologic complications of cancer and related disorders, and neurologic complications of therapy. The first year of training focuses primarily on the clinical aspects of neuro-oncology, whereas the second year of training focuses on research.
Core Areas for Training:
- Advanced principles in the diagnosis of primary and secondary nervous system malignancies
- Advanced principles in the management of primary and secondary nervous system malignancies such as:
- Primary CNS adult and pediatric tumors
- Metastatic cancer
- Metastases to the brain and spinal cord
- Leptomeningeal disease
- Metastases to peripheral nerves/plexus
- Metastases to base of skull
- Cancer related complications
- Encephalopathy
- CNS infections
- Cerebrovascular
- Seizures
- Elevated intracranial pressure
- Thromboembolism
- Neutropenia, thrombocytopenia, anemia
- Sepsis and other infections
- Metabolic disorders
- Pain management
- Palliative/end of life care
- Use of related chemotherapeutic agents, supportive medications related to neuro-oncology and blood products
- Recognition and management of complications related to chemotherapy and other therapeutic agents
- CAR-T cell neurotoxicity
- Neurotoxicity related to immunotherapy
- Neurologic side effects of chemotherapy

Curriculum
In addition to opportunities working in multidisciplinary ambulatory clinic sessions and evaluating inpatient consults, fellows are placed into continuity clinics and will be closely mentored by the Neuro-Oncology team. They are offered a range of educational sessions to supplement their clinical training such as:
- Introductory Lecture Series (July-September of 1st year of fellowship) with Hematology/Oncology Fellows
- Topics in Neuro-Oncology
- Clinical Journal Club
- Weekly Multidisciplinary Brain Tumor Board
- Neurology Grand Rounds
- Professional Development Series

Research
Following a clinically-heavy first year of fellowship, trainees spend the majority of their second year of fellowship devoted to research while maintaining their continuity clinics. A variety of research opportunities are available through the department of Neurology, Hematology/Oncology, Neurosurgery, Radiation Oncology, Pathology, and Radiology. Faculty members will meet with fellows early on in their clinical fellowship to discuss research interests and long-term career goals.
Fellows are also encouraged to apply for various research training opportunities across BIDMC and Harvard Medical School such as the Program in Clinical Effectiveness at Harvard T.H. Chan School of Public Health (link: Summer Program in Clinical Effectiveness 2022 | Harvard T.H. Chan School of Public Health<) and the Harvard Catalyst Clinical and Translational Research Academy (Clinical and Translational (C/T) Research Academy – Harvard Catalyst).
Supplementary courses on clinical research are available through Harvard Catalyst based on interest.
Teaching
For fellows who are interested in a career as a Clinician-Educator, mentored experiences are available. Scholarship didactics include the BIDMC Academy of Medical Educators (BIDMC Academy | BIDMC of Boston), the HMS Academy of Medical Educators (The Academy | Medical Education – Harvard Medical School), and the BIDMC Innovations in Media and Educational Delivery (iMED) Initiative.

Core Faculty
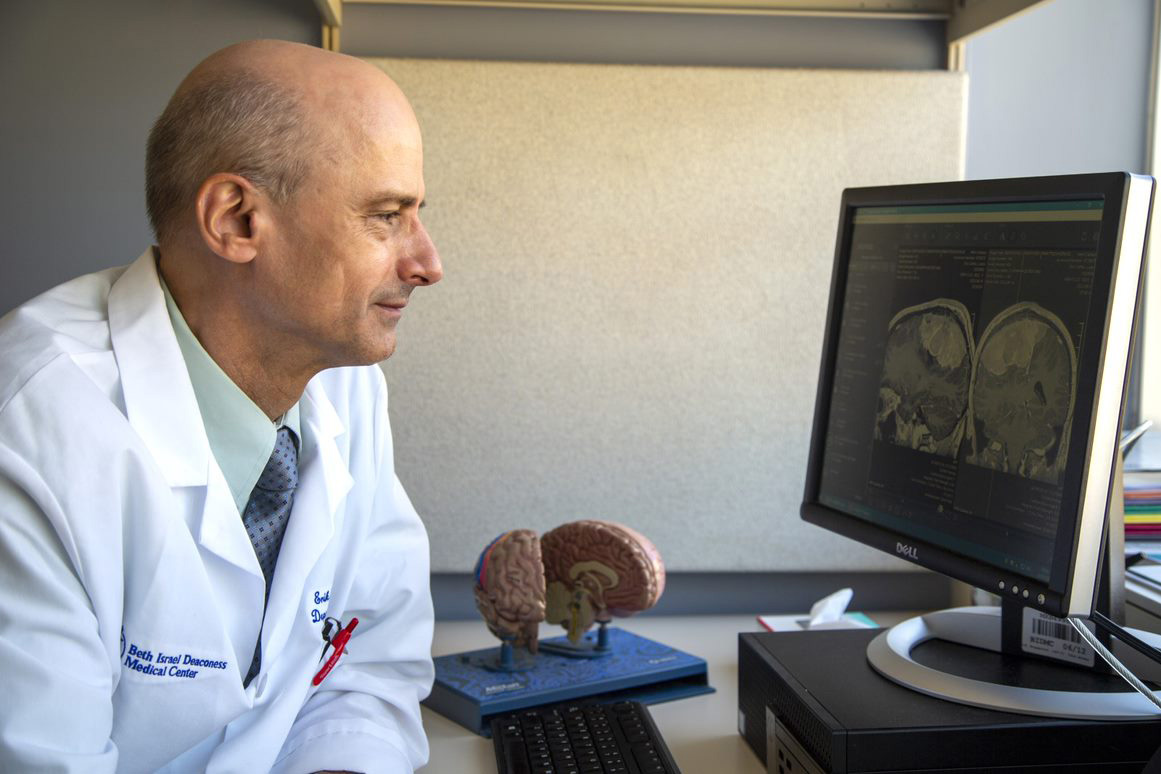
Neuro-Oncology
- K. Grace Ho, MD (Program Director)
- Erik Uhlmann, MD
Neurosurgery
- Rafael Vega, MD, PhD
Radiation Oncology
- Lauren Hertan, MD
Neuropathology
- Hemant Varma, MD
Neuroradiology
- Rafael Rojas, MD
How to Apply
We participate in the San Francisco Match Program (Overview – Neuro-Oncology Fellowship – SF Match – Residency and Fellowship Matching Services). Applicants should register with SF Match and send their application materials directly to SF Match, including a CV, short personal statement, and three letters of reference. Applicant registration begins November, and applications are due at the end of February. Interviews are offered between March-May. Please see the Neuro-Oncology Fellowship Timetable on the SF Match website for more specific dates, Match rules, and FAQs.
For questions about our program, please contact Billy Kanellopoulous at wkanello@bidmc.harvard.edu.
