About Our Fellowship
The Vascular Neurology Fellowship at BIDMC is ACGME accredited and involves both clinical training in the management of all cerebrovascular diseases and stroke, and the opportunity to participate in clinically related research for graduates of an accredited neurology residency program. There are three positions available each year, and the training is for a total of 12 months. However, interested fellows can reapply for a second year. In that case, their application for a second year will be considered on a case-by-case basis.
Our fellowship training provides complete exposure to:
- The problems of clinical stroke and other complicated cerebrovascular disorders
- Clinical stroke research
- Familiarity with clinical trials and methodology
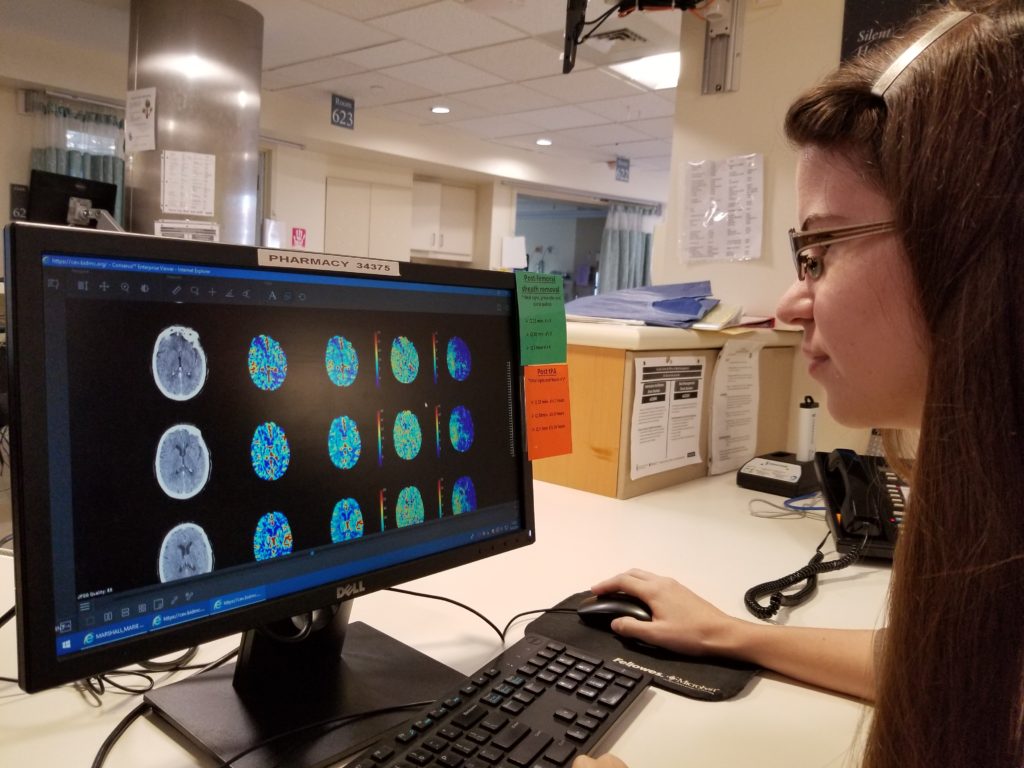
- Experience with the most recent advances in stroke technology
Overview
The Vascular Neurology Fellowship requires completion of at least 11 months of clinical services providing care to patients with cerebrovascular disorders and participation in an interdisciplinary team approach. Training includes clinical experiences in the:
- Outpatient stroke clinic
- Acute and inpatient stroke service
- Stroke consultation service
- Neurology Intensive Care Unit
- Telestroke
Training also includes exposure to neuroradiology and ultrasonography, as well as didactic lectures, stroke case conferences, and journal clubs. Elective opportunities at various related disciplines including rehabilitation, interventional neuroradiology, and research are also incorporated in the schedule.
We have strong collaborative services in Neuroradiology, Neurovascular surgery, Neuropathology, and Interventional Neuroradiology. There are more than 750 stroke patients admitted to our service each year and many more general cerebrovascular consultations. Our patient population provides an excellent clinical and research base. We have a computer-based stroke registry for ready access to our clinical materials. The stroke service is involved in many research projects including clinical trials for treatment of stroke and stroke prevention, and experimental trials of stroke recovery.
Interested applicants should contact Dr. Vasileios Lioutas (vlioutas@bidmc.harvard.edu) or Dr. Jennifer Dearborn (jtomazos@bidmc.harvard.edu) or call 617-632-8913 for more information.
Applications: Submit through ERAS
 Curriculum
Curriculum
The Vascular Neurology Fellowship Training Program pools the resources of the Departments of Neurology, Neurosurgery, and Radiology at Beth Israel Deaconess Medical Center.
The program’s primary goals are:
- The assessment of a Fellow’s competence shall serve as the basis for determining the minimum level of supervision required for different activities. Objective criteria to evaluate a Fellow’s progressive ability to function independently shall be developed and consistently applied. This assessment will include the evaluation of the Fellow’s communication skills, patient management, medical knowledge, and capacity to perform as required. The Program Director will communicate the assessment of the Fellow’s competence to the Fellow semi-annually, and when significant progress or deficiencies are noted.
- To provide the best possible training and education for the Fellows who pass through our program.
- To train individuals to become leaders in the field of Vascular Neurology, whether that is in the realm of clinical practice, clinical investigation, bench research, medical education or academic administration.
- To provide the Fellow with a strong curriculum about attitudes to care of patients with cerebrovascular diseases and the multi-disciplinary care of the patient.
The program teaches fellows how to provide patient care that is compassionate, appropriate, and cost/time effective. The fellow will be expected to make informed decisions regarding that care and provide and carry out management plans, counsel and educate patients and their families. Fellows completing our program should exhibit the highest possible levels of knowledge, clinical acumen and scholarship, and have the technical skills requisite for the practice of Vascular Neurology. They should observe the highest standards of professionalism and ethical behavior. We believe that our program is sufficiently different from other programs that our Fellows will stand out in any environment – practice or academic.
This curriculum describes in detail the individual components of the training program, grouped by the emergency department and inpatient consultations, longitudinal clinics in vascular and general Neurology, elective exposures, research, and didactic sessions/conferences.
Revision of the Curriculum
This curriculum is subject to revision by the stroke faculty members, incorporating fellows’ feedback to keep it current, relevant and in accord with ACGME Resident Review Committee (RRC) requirements. The program has adopted a style of continuous improvement, implementing reasonable strategies and discarding those that are not providing the expected benefit, after a period of application and evaluation. The Beth Israel Deaconess Medical Center Training Program in Vascular Neurology is an ACGME-approved program. As part of the regular process of RRC approval by the ACGME, this curriculum is also subject to RRC approval.
Fellowship Duties
Emergency, Acute inpatient and Neurologic Intensive Care Unit duties
Each fellow spends a minimum of 4 months on the acute and inpatient stroke service. The three fellows will alternate being on service, one week at a time. While on service, the fellow will participate in the daily rounds on the Neurology patients in the Neuro ICU and the inpatient stroke service. They are required to be familiar with all aspects of the individual patient’s care, but may delegate case presentations to the Neurology residents. While the Neuro ICU team and Neurology resident assume direct patient responsibility, the fellow will be required to supervise and teach the Neurology resident (who also writes detailed daily progress notes). The chief residents will have direct patient responsibility, under the supervision of the attending, for patients on the inpatient stroke service. In all cases, the fellow will serve as an adjunct to the attending with responsibilities delegated as the attending sees fit.
The on-service fellow will respond to Stroke Pager calls during weekdays and nights and weekends, when on service, and provide 24-hour coverage for the acute stroke service, including urgent Emergency Department evaluations and inpatient consultations, with individual case review for each case by the attending.
The on-call fellow also responds to Telestroke calls after hours (5pm-8am) during week days and during weekends, along with the on-call attending.
For the off-service weeks the fellows spend one week covering the Telestroke service (8am-5pm) on weekdays and covering the Neurosonology service and another week on research and elective time.
Telestroke
Our service currently covers 7 satellite hospitals for Telestroke services. The fellows are the first responders, triaging all incoming calls and determining the need to escalate to a full video consultation which is completed with the participation of the on-call attending via a virtual platform.
Outpatient clinic
Each fellow attends one half-day clinic session during his/her off-service weeks under the supervision of a stroke service attending. The clinic will consist primarily of stroke patients (new and follow up from inpatient hospitalization). However, on occasion, unoccupied slots may be given to general neurology patients.
Elective and research
The fellows will have a total of 4 months dedicated to electives and research. The time allocated to each of the two components is flexible and dependent on the fellow’s level of engagement in individual research activities.
Electives are designed to complement the fellows’ experience with aspects of Vascular Neurology that are not traditionally encountered in the main inpatient and outpatient rotations. Fellows can choose from the following electives: Post-stroke spasticity management, Cognitive Neurology and Neurorehabilitation, Interventional Neuroradiology, Vascular Medicine (focus on non-cerebrovascular arteriopathies, management of systemic atherosclerosis in the Vascular Medicine clinic), Pediatric Stroke (at the Children’s hospital).
For research, there are options for involvement in ongoing multicenter clinical trials and independent or joint original research. For further details see the segments below “Our Research and Clinical Trials” and “Research and Publications” under “Additional Information”.
Goals and Objectives
During the one-year training, fellows will be expected to progressively gain the knowledge and skills necessary for the diagnosis and management of a wide range of cerebrovascular diseases and others that result in vascular injury to the nervous system. The primary goal is for the trainee to be capable of independently managing any type of clinical situation related to stroke.
The overall objective for our Vascular Neurology fellowship training program is to provide the trainees with the skills and knowledge necessary to:
- Provide high quality clinical care and assessment of patients with various cerebrovascular disorders in different settings (Emergency, inpatient, and outpatient), including diagnostic evaluation, treatment, management, counseling and prevention.
- Management of critically-ill neurological patients, such as those with cerebral hemorrhage, brain aneurysms or vascular malformations, head trauma, brain tumors, status epilepticus, myasthenic crisis, and Guillain-Barre syndrome.
- Work effectively with multidisciplinary teams oriented to the care of these patients.
- Ordering and interpretation of laboratory and imaging tests in patients with cerebrovascular diseases and stroke
- Develop the capacity to pursue an academic career in the field of stroke and cerebrovascular disorders.
Clearly, the goals during any given rotation will depend on the rotation. During ultrasound neck and TCD, performance and interpretation will be emphasized. During neuroradiology, other imaging techniques will be emphasized. In the clinic, consultative rotations clinical details and evaluation will be prominent, and in the emergency room rotation, rapid evaluation and treatment will take precedence.
The specific goals and objectives of the cerebrovascular fellowship training are:
- To become familiar with the clinical syndromes in patients with brain ischemia and hemorrhage.
- To know the basic anatomy, pathology, and pathophysiology of the cerebrovascular system and the relevant cardiac and hematological systems.
- To become very familiar with the important cerebrovascular disease literature.
- To learn in depth the important therapeutic options, their indications, potential benefits and risks.
- To become skilled in weighing benefits vs risks in making therapeutic decisions.
- To become capable in interpreting the various cerebrovascular investigations: CT scanning, MRI, MRA, CTA, standard dye angiography, cervical ultrasound of the carotid and vertebral arteries, and transcranial Doppler.
- To become skilled at rapid evaluation of patients with acute stroke syndromes.
- To be able to tell patients their problems in a sensitive and clear fashion and to improve all interpersonal skills.
- To understand basic research techniques.
- To understand the major issues in cerebrovascular disease that already have been answered successfully and the conundrums and uncertainties that remain.
- To learn how to design, plan, and carry-out research projects.
- Become familiar with biostatistical analyses of randomized trials.
Fellow Responsibilities
The trainee’s mandatory duties and responsibilities include:
- Evaluation of acute stroke patients in the Emergency Department.
- Participation in Telestroke consultations under direct supervision of an attending.
- Supervise acute care of stroke patients (on the inpatient stroke service) and critically ill stroke patients (in the Neuro ICU) in the inpatient setting.
- Have two outpatient clinic sessions every other week.
- Learn and interpret diffusion- and perfusion-weighted MRI and MRA; and perfusion CT and CTA.
- Learn and perform, under supervision, transcranial Doppler studies.
- Alternate organizing a weekly stroke conference, and attend all weekly stroke conferences.
- Alternate night call to provide 24/7 coverage for code stroke, on a weekly basis.
- Participate in the ongoing clinical trials involving stroke patients.
- Enter patients’ data into our computerized stroke registry on a weekly basis.
- Completion of NIHSS and mRS training and certification during the first 2 weeks of training.
- Completion of the CITI Human Subject Training Curriculum and HIPPA tutorials and exams offered at BIDMC during the first 2 weeks of training.
- Teaching medical students and residents during daily rounds.
The trainee is required to maintain a log of patients evaluated throughout his/her training with regard to clinical diagnosis to assure that the diversity of cerebrovascular disorders cases has been seen and that an understanding of the condition has been achieved.
Hours of Work and Call Schedule
Generally, daytime business hours with night call, when on service. Each fellow will be on call for a total of 4 months. Night call is from home with a neurology resident in-house to help get things started while the fellow makes his or her way in. A stroke service attending is always available for back up consultation, and to discuss each patient with the fellow and to review the examination and neuroimages. The three fellows will alternate being on-call for one week at a time every third week. We expect the fellows to be flexible and in general, available to switch when something ‘suddenly comes up’.
In the rare instances where only one fellow is accepted into the program, the fellow will be on service 5 days per week (Monday 8 a.m. to Friday 5 p.m.), with 4 night calls. The fellow will be guaranteed 2 days (weekend) every week away from the hospital. The general Neurology Chief residents will provide coverage for the other nights, under direct supervision of the stroke service Attending Physicians.
Additional Information
Research and Publications
We encourage supervised, independent or joint, stroke-related research during the fellowship. The fellow will be offered the opportunity to assist in the preparation and submission of articles in peer-reviewed journals. Authorship will be commensurate to the proportion of involvement in the intellectual planning of the paper and the work done in gathering and entering the data. Our goal is to have each fellow as a first author on at least one publication by the end of the fellowship, and to present at least one abstract at a scientific meeting during or shortly after fellowship.
Scientific Meetings and Travel
Fellows are encouraged to attend at least one educational conference during their one year of training. Attendance at the AHA/ASA Stroke Conference and the European Stroke Organization Conference, where the fellows get an opportunity to interact with renowned Cerebrovascular experts, is advised. We expect the three fellows to alternate attendance at these meetings or not to attend the same meeting to avoid interruption of our 24/7 stroke coverage.
Supervision
The fellows will be directly supervised by one of the stroke attendings at all times during their inpatient, outpatient, or elective rotations. Feedback will be provided directly and immediately to the fellow by the attendings. In addition, our division meets weekly to review programmatic issues and fellows’ activities and performance. Our division maintains an open door policy: Fellows are encouraged to discuss their concerns, stresses, challenges and plans with any of the stroke attendings at any time.
Vacation and Benefits
Fellows usually receive three weeks of paid personal vacation per year, in addition to one week to attend scientific meetings and conferences, if needed. We prefer taking one week off at a time, but longer vacation periods can be arranged if necessary. Schedules may be adjusted around the holidays or long weekends, if needed.
Salary
Fellowship stipend varies depending on the PGY level. This is usually adjusted by the hospital on a yearly basis to adjust for changes in cost of living.
Moonlighting
Moonlighting during the Cerebrovascular fellowship training is strictly prohibited.
The Neurology Department at BIDMC offers an ACGME-accredited fellowship in stroke and cerebrovascular disease. Fellows serve on the stroke service and supervise residents in the Neuro-ICU where they receive training in the latest treatment advances for a full range of neurological conditions, including stroke and ICU neurology. A didactic stroke conference and case presentation is held weekly every Thursday at 4 p.m.

