Training Sites
Beth Israel Deaconess Medical Center
Beth Israel Deaconess Medical Center (BIDMC) has two campuses on opposite sides of Brookline Avenue (East Campus and West Campus). The Neurology/Neurosurgery inpatient wards and Neuro ICU are on the West Campus, along with the Emergency Department, most acute medical and surgical services, and the in-patient Psychiatry ward. The East Campus houses several medical and surgical specialties, a Medical ICU, Obstetrics-Gynecology, and Oncology including the bone marrow transplant unit. In addition, most outpatient facilities including the Neurology Ambulatory Clinics in the Shapiro Clinical Center are on the East. The Department of Neurology provides consultation services on both campuses.
Boston Children’s Hospital is one of the leading Children’s hospitals in the world; it is located a few yards from the BIDMC East campus. All Child Neurology rotations are there, and many residents share the extensive research facilities at BCH, as well.
Spaulding Rehabilitation hospital in Cambridge is utilized for several days of Rehab Neurology during the Rehab rotation, supervised by our Cognitive Neurology group.
PGY-2 (Junior Year)
During the first year, residents take primary responsibility for the care of inpatients on the Neurology ward services at BIDMC and Children’s Hospital and in the Neuro ICU at BIDMC. At Beth Israel, the Neurology ward includes both the General Neurology and Stroke services. The General Neurology service is the “heart and soul” of diagnostic Neurology, serving patients with common and some very unusual illnesses: from gait disorder to new cases of multiple sclerosis, mass lesions of unclear nature, demyelinating diseases of the central or peripheral nervous system, rapid-onset cognitive loss, neurologic infections, etc. It also covers Epilepsy patients, with a separate attending and fellow, but the same residents/student team. The Stroke service (perhaps the “heart and vessels”) evaluates and treats a large number of patients with vascular problems, mostly ischemic and hemorrhagic strokes. Here, residents learn Neuroanatomy and localization by neurologic examination, as well as gaining expertise in reading sophisticated neuroradiologic studies. On each team, the chief resident leads 2 junior residents and usually, 2 HMS students. At Childrens’ Hospital the ward is half Epilepsy, half General Neurology.
Junior residents spend 8 weeks (in 4 blocks; Monday to Friday; 7a.m. to 7 p.m.) in the Neuro-ICU at BIDMC where a multidisciplinary team takes care of acutely ill Neurology and Neurosurgery patients. Residents round in the Neuro ICU with the Stroke team on acutely ill stroke patients.
In Neurophysiology rotations, residents learn the principles of EEG and epilepsy; EMG and neuromuscular disease; and Sleep Neurology. In the Neurorehabilitation block, residents spend time at a Rehab hospital (Spaulding) under the supervision of neurologists with special training in Rehabilitation Neurology, and also in the Cognitive Neurology clinics at Beth Israel, seeing patients with head injuries, cognitive and behavioral problems, and after strokes, etc. The Psychiatry month can be on the Psychiatry ward or Consult Liaison service.
Call: on the wards is q4. ‘Short call,’ Sunday to Thursday, ends at 8pm (no overnight call during the week); overnight Friday and Saturday (1 each / month), going home immediately after rounds the following morning and off for the remainder of the weekend.
The Night Float resident covers the Neurology wards, 8 pm to 8 am, Sunday through Thursday, to ensure that ward residents get adequate sleep and time off. Night Float is covered by senior residents the first half of the year and by junior residents the 2nd half. In addition, there is an in-house PGY-3 or 4 resident covering the Emergency Department 7 nights per week, available to support the Night Float or junior resident, as needed. Night call at Children’s Hospital in the junior year is every 4th night, leaving after rounds in the morning. Neurophysiology, Neurorehab / Cognitive, SubSpecialty clinics, Psychiatry, and electives have no night call, but there is occasional weekend ED coverage.
Work hour limits are observed strictly. Residents are always be scheduled to work < 80 hours / week and have at least 1 day in 7 completely off, averaged over a 4 week period. The scheduling chief residents attempt to schedule juniors on Wards + ICU + NF for no more than 6 – 8 weeks in a row.
PGY-3 (Senior Year)
During the senior year, residents learn to be Neurology consultants, rotating on consultation services on the East and West Campuses of BIDMC and at Children’s Hospital. Many urgent consults are evaluated in the Emergency Department rotation, including seizures, rapidly progressive weakness, and Code Stroke activations — where the Vascular Neurology fellows and residents play a key role in the administration of tPA and help facilitate mechanical thrombectomy (there are roughly 100 thrombectomy cases at BIDMC every year).
Consultations at Children’s Hospital include one month on the general inpatient consult team and another on the ICU-specific consult team. The Children’s ICU rotation is one of the more demanding rotations but also one of the most interesting and educational — providing the opportunity to hone EEG skills, care for patients with rare genetic diagnoses, and develop a comprehensive understanding of the spectrum of neurologic disorders across the lifespan.
In addition to broadening their exposure to a wide variety of clinical Neurology, senior year residents develop research projects, finalize career goals and apply for fellowships. Study abroad opportunities are also available, particularly the month in Zambia.
Call: Senior residents cover the Night Float schedule in the 1st half of the year. The Night Backup provides support to the juniors and NF residents in the ED at night. The Emergency Department rotation has no overnight call but includes some weekend days. There is no night call in the Neuro ICU.
PGY-4 (Chief Year)
During the Chief year, residents have much greater autonomy and learn to make clinical decisions and lead teams independently (always with faculty backup). PGY-4 residents serve as the Chief Residents on both the Stroke and General/Epilepsy services. They take primary responsibility for coordinating rounds, supervising the junior residents, and teaching the medical students. Chief residents take report on all new admissions and consults after 5 PM, building the experience and confidence required of an independent neurologist. Emergency Dept coverage is 11 am to 7 pm, weekdays.
The chief year is also a time for scholarship (whether basic investigations, clinical research, or education projects, etc.) to begin and refine individual career paths. For clinician scientists, the NIH-sponsored R25 research grant entails a 6 month block, with some elective time moved from PGY3.
Chief Residents spend 4 weeks on a Neuropathology rotation, preparing cases for Neuropathology conferences and teaching their fellow residents high-yield topics. They may spend 2 months as teaching assistants in Neuroanatomy for pre-clerkship medical students in the “Mind, Brain, and Behavior” course at Harvard Medical School. The remainder of the year includes sub-specialty clinics and elective time for research, teaching, and other projects.
Call: Chief residents on the General Neurology and Stroke services take call from home (alternate nights and half the weekends) advising in-house residents on ED cases, admissions, and consults, and backing up junior and NF residents in the ED at night for about 2 weeks.
Rotations by Year (weeks)
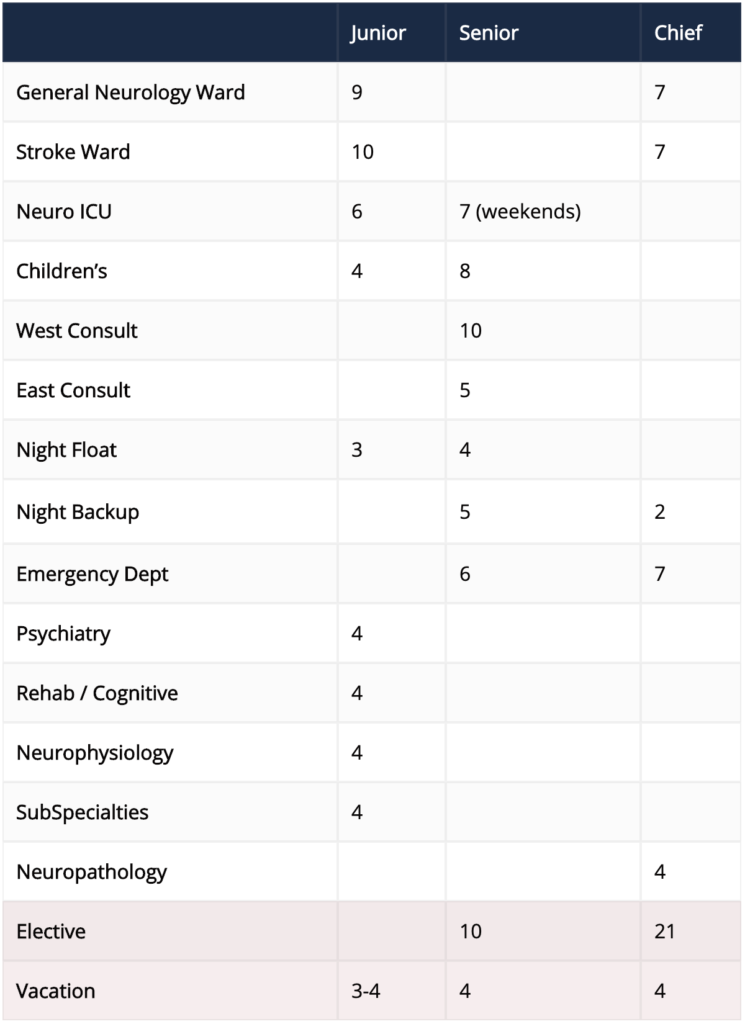 *These schedules are approximate; individual schedules may vary.
*These schedules are approximate; individual schedules may vary.
Outpatient Experience:
With a wide breadth and depth of outpatient experiences, BIDMC residents follow their own continuity patients for 3 years, as well as evaluating patients in several different subspecialty clinics.
Continuity Clinic:
The outpatient Neurology experience centers in the Neurology continuity clinics. At the beginning of the PGY-2 year, each resident is assigned a clinic with an attending neurologist at BIDMC with whom s/he sees General Neurology patients every other week for the 3 years of residency. In the first year, this is paired with a Child Neurology clinic at Boston Children’s Hospital, alternate weeks. After that year, the Child Neurology clinic is replaced by a second adult Neurology clinic with a second attending neurologist at BIDMC, continuing for the remainder of residency. The longitudinal relationship with the clinic attendings facilitates comprehensive guidance and evaluation of the resident’s growth over time and for mentorship.
Specialty Clinics:
In the Subspecialty Clinic rotation of the junior year, residents evaluate conditions seen less frequently on the wards, including Multiple Sclerosis, Movement Disorders, Cognitive Neurology, Neuro-Oncology, etc. [Many residents want experience in these areas well before making decisions about fellowships.] Junior residents also participate in a Neurophysiology block, with clinics and physiology testing in Epilepsy (EEG), Neuromuscular Disorders (EMG), and Sleep Neurology (with sleep studies). In the Neurorehabilitation rotation, residents see inpatients recovering from acute neurologic illnesses (such as head injury and strokes) at the Spaulding Hospital Rehabilitation Center and outpatients with cognitive and behavioral problems in the Cognitive Neurology clinics.
During the 2nd and 3rd year elective blocks, residents have their choice of subspecialty clinics. Popular clinics among residents include Neuro-ophthalmology, Neuroimmunology/MS, Movement disorders, Neuro-oncology, Headache, Autonomic disorders, Epilepsy, Neuromuscular disorders, Sleep disorders, and Neuro-ID. For residents with a particular interest in the field, there an option for a longitudinal Movement Disorders clinic for 6 months in the chief year with Dr. Samuel Frank.
BIDMC Neurology Teaching Awards:
 Michael Ronthal Award
Michael Ronthal Award
This award is given to a graduating resident who has distinguished themselves as an outstanding educator.
2023 – Ari Axelbaum
2022 – Brandon Merical
2021 – Jonah Zuflacht
2020 – Erika Sigman
2019 – Charles Casassa
2018 – Kathie Lin
2017 – Alana Kirby
2016 – Marc Bouffard
2015 – Bart Chwalisz
2014 – Simon Laganiere
2013 – Nigel Pedersen
2012 – Aimee Boegle
2011 – Soma Sengupta
Outstanding Teacher Award
This award is given to a faculty member on behalf of the graduating class in recognition of outstanding teaching and mentorship.
2023 – Clifford Saper
2022 – Corey Fehnel
2021 – Bernard Chang
2020 – Jennifer Dearborn-Tomazos
2019 – Gottfried Schlaug
2018 – Michael Ronthal
2017 – Sam Frank
2016 – Pushpa Narayanaswami
2015 – Nurhan Torun
2014 – Michael Alexander
2013 – Rolf Pfannl
2012 – Sandeep Kumar
2011 – Gottfried Schlaug
2010 – Louis Caplan
2009 – Andrew Tarulli
2008 – Penny Greenstein
2007 – Daniel Press
2006 – Sean Savitz
